Building Bridges with Private Hospitals in Thiruvananthapuram
On 23rd November, as a part of the Community-Based Palliative Care (CBPC) project, we conducted a sensitisation and orientation session for private hospitals in Thiruvananthapuram, with the aim of initiating conversations around integrating palliative care into routine healthcare services. What appeared on paper as a straightforward orientation programme soon became a deeply instructive journey in persistence, relationship-building, and faith in the process.
As part of the initial planning, we reached out to 24 private hospitals across Thiruvananthapuram. From the beginning, one of the biggest challenges was the level of participation we were hoping for. For meaningful institutional integration, it was important that decision-makers such as MDs, CEOs, CMOs, and senior management representatives were part of the conversation. Reaching this level of leadership, however, was far from easy.
The programme was scheduled on a Sunday, which further complicated matters, especially given the nature of corporate hospitals where weekends are often tightly structured or reserved. The initial responses were largely discouraging. Many hospitals were non-committal, some were unreachable, and others politely declined. At several points, it genuinely felt like the programme might not take shape at all.
Connecting with hospital leadership turned into a process that demanded patience and persistence. I found myself repeatedly following up with MDs, CEOs, CMOs, PROs and administrators through calls and messages, often across different times of the day, regardless of weekdays or weekends. Even up to the day before the programme, a few confirmed participants informed us of their inability to attend, adding to the uncertainty and emotional weight of coordination.
It was on that day, sensing my growing anxiety and exhaustion, that Dr. M. R. Rajagopal gently reassured me. He said that even if only five hospital representatives turned up, we would still go ahead with the meeting and consider it a success. That moment of reassurance, grounded in experience, calm, and faith in the process, offered immense comfort and reminded me that the value of such work does not lie in numbers alone, but in intent and sincerity.
Yet, this journey also reaffirmed something essential about community work: relationships matter, and persistence often opens doors that formal communication cannot. With the steady support of hospital PROs, doctors, and key individuals, including Dr. M. R. Rajagopal, Community Social Officer Gokul, TIPS Executive Director Manoj, TIPS Director Dr. Sunil, Dr. Arjun, and Dr. Aakash, we were eventually able to establish direct administrative-level contact with 14 hospitals. On the day of the programme, 23rd November, despite all the challenges leading up to it, representatives from 13 hospitals attended. What unfolded was both surprising and deeply heartening. As participants kept arriving, we found ourselves bringing in more and more chairs to accommodate everyone. The room gradually filled beyond our expectations, quietly transforming our anxiety into relief and gratitude. What stood out was the level of leadership present. CEOs, MDs, CMOs, PROs, and quality control team members took part, which itself felt like a significant achievement. Their presence reflected a willingness to engage seriously with the idea of strengthening palliative care within institutional systems.
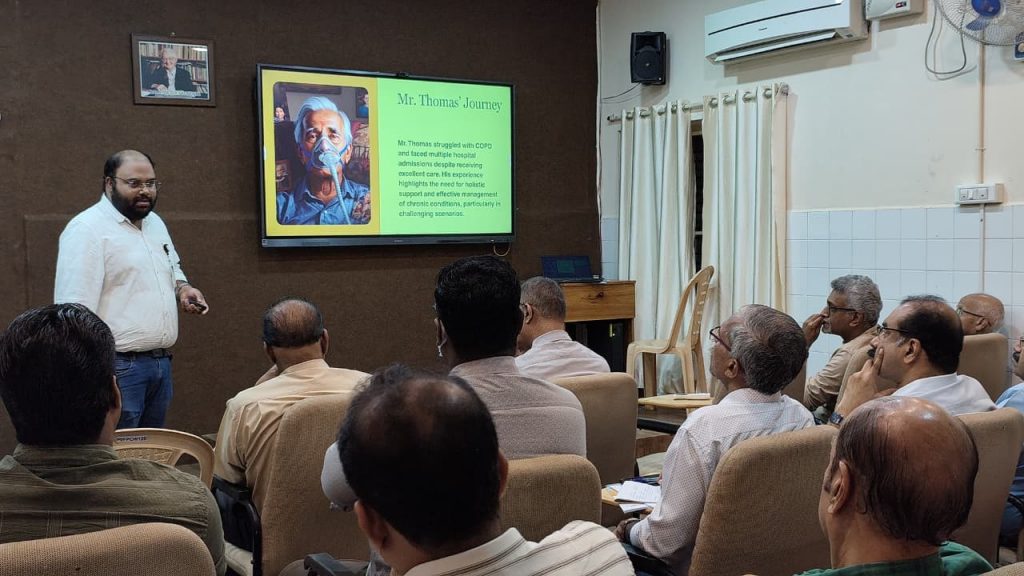


A two-hour interactive session was conducted with doctors, focusing on the relevance, scope, and practical pathways for integrating palliative care into hospital services. The discussions were thoughtful and encouraging. Participants raised questions, shared their institutional concerns, and spoke openly about the gaps and possibilities they saw within their own settings. There was a genuine curiosity and openness that made the session deeply affirming.
As part of the programme, we also introduced a structured questionnaire designed to assess each hospital’s level of interest, readiness, and tentative timelines for engagement. This tool has since helped us streamline post-meeting follow-ups in a more focused and systematic manner.
What was especially heartening was what followed. Six hospitals proactively reached out after the session, expressing interest in further collaboration. Direct follow-up meetings have already been completed with two institutions — Parvathy Hospital and Panavoor Marian Hospital. Additionally, CSI Karakonam Hospital has planned to conduct a dedicated palliative care–related programme on 7th January 2026, marking a tangible and hopeful outcome of this initiative.
Looking back, this experience reinforced an important lesson for me as a community social worker: meaningful systems change rarely comes easily. It requires repeated engagement, patience in the face of silence, and a willingness to keep showing up even when outcomes feel uncertain. This initiative reaffirmed that consistent follow-up, personal connection, and trust-building can gradually bring institutional leadership on board.
The encouraging responses and emerging collaborations give us hope that palliative care can find a stronger, more rooted presence within private healthcare institutions in Thiruvananthapuram. This journey, though challenging, has been deeply affirming, reminding me why community-based work, grounded in persistence and relationships, continues to matter.

Shijo Kurian Thomas
Community Social Officer, Pallium India






