Why oral morphine is out of reach…
Oral morphine is not available; but transdermal fentanyl is. The latter is 150 times more expensive than ordinary morphine tablets and less suitable for starting management of pain.
Why is the affordable simple medicine not available? And why is the expensive one available when they are both covered by the same regulations? This was one of the several issues related to low and middle income countries that were brought up in a webinar ‘Eastern Comparative Models in Palliative Care: Perspectives from Africa, Asia, and the Americas’.
The event was part of the ‘afterlife’ of the Lancet Commission on Palliative Care and Pain Relief (2018), which discusses access to palliative care.
Read the report here: The Lancet Commission on Palliative Care and Pain Relief—findings, recommendations, and future directions – The Lancet Global Health
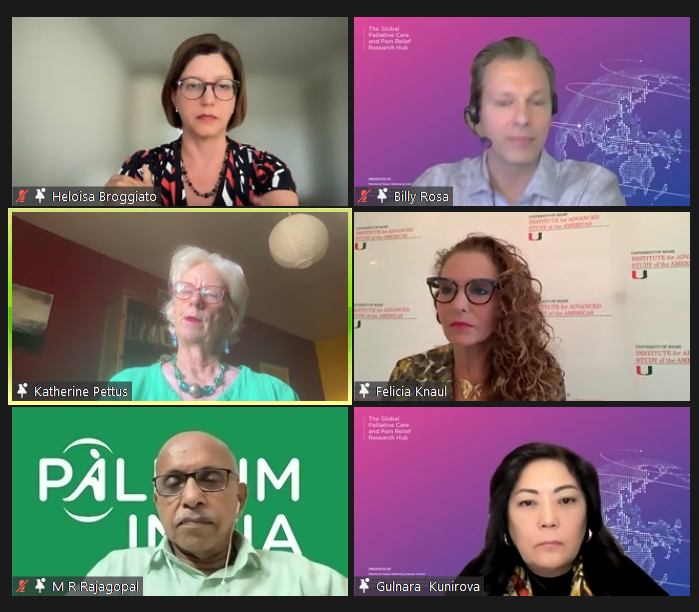
Global palliative care champions shared updates on the progress made in the field in their regions, revealing each had made advances and lags in different aspects. In a recent webinar organised by the Global Palliative Care and Pain Relief Research Hub, participants shared progress and problem areas in their regions.
Experts who shared updates include Heloísa Broggiato Matter from the United Kingdom, Gulnara Kunirova from Kazakhstan, Emmanuel Luyirika and Eve Namisango from Uganda, Dr M.R. Rajagopal from India, and Katherine Pettus, Felicia Knaul and Billy Rosa from the US.
Emmanuel and Eve, who gave an overview of palliative care access in Uganda and surrounding region, stressed on the need for more education and wider practice of the speciality.
Gulnara gave an overview of palliative care access in Kazakhstan and surrounding region, sharing ideal models and progress made with public-private partnerships, as well as commendable work by non-profits in the field.
Heloisa gave a glimpse of the palliative care access in Brazil and surrounding region, expressing concern about pain medicine access in most parts. She explained how the involvement of drug mafia was resulting in shortage of essential pain medicines.
Dr Rajagopal gave an overview of policy and practice priorities in India and the region. He said it was high time for global palliative care professionals to realise the potential and reach of involving local communities in the palliative care network if they hoped to push the unruly elephant, namely illness related suffering, posing an ominous threat at the centre of healthcare sector.
The webinar was organised to discuss global palliative care and pain relief access to alleviate serious health-related suffering worldwide, structural and system-level barriers that prevent universal access to palliative care as a component of universal health coverage, recognize public and global health inequities in palliative care and pain relief and actionable methods to promote social justice, and to identify national and global advocacy efforts and opportunities to increase palliative care and pain relief access across contexts and clinical settings.